WASHINGTON, DC - The Subcommittee on Oversight and Investigations, chaired by Rep. Tim Murphy (R-PA), today held a hearing examining waste, fraud, and abuse within the Medicare and Medicaid programs. Officials from the Centers for Medicare and Medicaid Services (CMS), U.S. Government Accountability Office (GAO), and HHS Office of the Inspector General (OIG) testified.
“Just last year, HHS estimated approximately $89 billion dollars in improper payments through Medicare and Medicaid," stated Chairman Murphy. “This means that the federal government cannot verify the accuracy of one out of every ten payments."
Chairman Murphy raised questions with the panel about site visits to verify providers, specifically flagging for Dr. Shantanu Agrawal, Deputy Administrator and Director, Center for Program Integrity at CMS, incidents when officials conducted site visits and issued reports saying they did not meet standards to qualify as a provider, yet half of these “providers" enrolled into the official Medicare provider database anyway. Dr. Agrawal responded by acknowledging that “there are elements of the process that need to be changed."
Later in the hearing, Chairman Murphy followed up on the provider site visits. CMS has issued guidance limiting on-site verification by contractors, but a GAO report cautioned this could increase the potential for fraud.
Seto Bagdoyan, Director of Audit Services, Forensic Audits and Investigative Service at GAO, pointed out why solely relying on raw data is not enough, and that boots on the ground and criminal investigators are needed. He testified, “Well if you dial back the verification steps, and you can essentially meet the new guidance by picking up the phone, dialing a provider and asking them ‘is this your address’ and the provider says ‘yes,’ then you leave it at that, that obviously is potential concern." Ann Maxwell, Assistant Inspector General at HHS’ OIG, also emphasized the importance of CMS fully implementing and maximizing tools designed to prevent unscrupulous providers from enrolling into Medicare, such as enhanced provider screening.
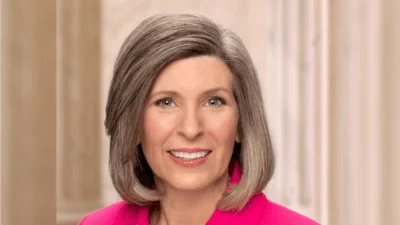
Rep. Susan Brooks (R-IN) highlighted the number of reports focused on Medicare and Medicaid fraud over the last 10 years, saying, “It truly is astonishing that after 10 years of albeit thoughtful reports - many reports - we’ve continued to allow our nation’s largest health insurance programs to run really with this much fraud for this long of a period of time. But I’m encouraged that we’re continuing as a subcommittee for answers that protect beneficiaries as well as taxpayer dollars."
Chairman Murphy concluded the hearing by echoing Ranking Member Diana DeGette’s (D-CO) interest in holding a follow-up hearing to measure CMS’s progress in one year.
Additional information on today’s hearing, including a background memo, witness testimony, and an archived video can be found on our website here. Related Items
* Medicare and Medicaid Program Integrity: Combatting Improper Payments and Ineligible Providers