Dear Dr. McClellan:
We are writing to express our concern regarding the Centers for Medicare and Medicaid Services (CMS) proposed changes to the Long Term Care Hospital (LTCH) prospective payment system. Taken together, the proposed changes would result in an estimated 14.7 percent decline in Medicare payments to LTCHs in 2007.
The Federal government has a duty to taxpayers to pay appropriately for the right care in the right setting. LTCHs provide post-acute care to a relatively small number of medically complex patients. The rapid growth in the number of LTCHs and the significant increase in Medicare’s spending on these providers have highlighted a need to more closely examine the LTCH payment system, and we are pleased that CMS is doing so.
Yet, CMS has advocated far-reaching changes in LTCH payment policy for the coming year, including significant modifications to the short stay outlier policy. A short stay outlier is defined as a patient whose length of stay is less than or equal to 5/6 of the geometric mean length of stay for the diagnosis-related group (DRG). Currently, payment for short stay cases is the lesser of: 1) the full LTCH DRG payment rate; 2) 120 percent of the LTCH DRG per-diem rate; or 3) 120 percent of the cost of the short stay case. In its rule, CMS proposes to reduce payment in the third category from 120 percent of cost to 100 percent of cost, and to add a new criterion: 4) payment comparable to the acute care hospital inpatient DRG rate.
We are concerned that this proposed short stay policy is too severe. It would affect over a third of LTCH cases, and could pay providers significantly below the reasonable cost of caring for these patients. Patients treated in LTCHs are typically much sicker than those treated in general acute care hospitals, and are thus likely to require more resources. While we share the Agency’s concerns about the rapid growth of LTCHs, we do not believe that CMS’ rationale for paying short stay cases at the acute care rate is justified by the data.
Additionally, this policy does not address the underlying concern of potentially inappropriate patient admissions to LTCH facilities. We encourage CMS to expeditiously develop for public comment patient and facility criteria to ensure that only appropriate patients are utilizing LTCH services. We support the Medicare Payment Advisory Commission’s recommendations in this area, and would support the development of admission standards and discharge criteria. We urge CMS to continue its efforts to develop a more accurate means of classifying post-acute care patients, and we look forward to working with you to that end.
Thank you for your consideration of these concerns.
Sincerely,
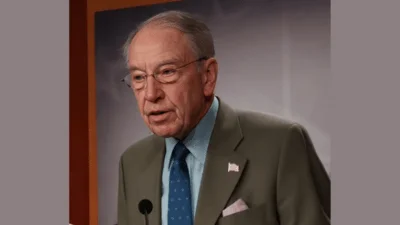
Charles E. Grassley
Chairman
Max Baucus Ranking Member
Orrin Hatch
John D. Rockefeller Trent Lott
John Kerry Rick Santorum
Blanche Lincoln Jim Bunning
Ron Wyden Charles Schumer
Source: Ranking Member’s News