Dear Administrator Tavenner:
The Supreme Court will soon consider the legality of regulations extending Advanced Premium Tax Credits (APTCs) to insurance policies purchased in the federally-facilitated marketplace, HealthCare.gov. These regulations were promulgated despite statutory language extending APTCs only to insurance policies enrolled through state-based exchanges. This action, which violated the Executive Branch’s statutory authority, sought to expand the reach of APTCs and employer mandate penalty taxes to approximately 4 million HealthCare.gov enrollees and 250,000 employers, respectively. Should the court rule against the Administration, these 4 million people will likely lose their illegal subsidies, could see their insurance bill quadruple, and may lose their health insurance policies.
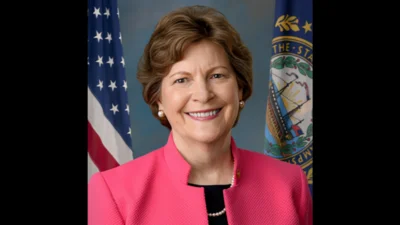
Rather than educating HealthCare.gov enrollees about this possibility or planning for a possible adverse ruling, the Administration has publicly insisted that the Supreme Court case does not pose a risk to HealthCare.gov subsidies, not does it merit contingency planning. In a recent hearing before the Committee on Finance, Health and Human Services Secretary Sylvia Burwell insisted that her “focus is on completing and implementing the law," and that her sole focus “is the open enrollment." Statements by the White House, the Justice Department, Secretary Burwell, and you have all repeated the phrase that “nothing has changed" in light of the lawsuit.
But the Administration’s actions behind closed doors tells a different story. While the Administration assures HealthCare.gov policyholders that “nothing has changed," it has been conveying a contradictory message to health insurance companies. Late last year, CMS altered the agreements to participate in the federal exchange, guaranteeing insurance companies the right to pull out of their contracts should federal subsidies such as the APTC come to an end - in other words, if the Administration loses before the Supreme Court. The agreement included a termination clause with the following language:
CMS acknowledges that [the insurer] has developed its product for the [federal exchange] based on the assumption that APTCs… will be available to qualifying Enrollees. In the event that this assumption ceases to be valid during the term of this Agreement, CMS acknowledges that Issuer could have cause to terminate this Agreement….
CMS officials told media that the new termination clause was added at the request of insurers, and that both insurance companies and CMS thought it was “critical." The Administration accommodated insurers with this “critical" change at the same time it was telling individual Americans that “nothing has changed," suggesting that the Administration is both actively engaged in contingency planning and is misleading HealthCare.gov enrollees.
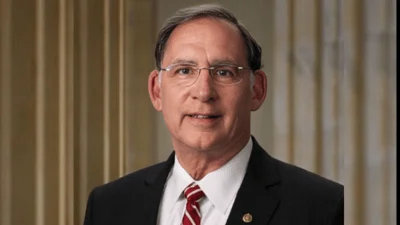
As Chairman of the Senate Finance Committee, which oversees both the activities of your agency and that of the Internal Revenue Service which issued the underlying regulations, I have the duty to conduct oversight on this matter. To assist me in carrying out this duty, I ask that you provide the following documents and information by no later than March 6, 2015. The relevant time frame for all document requests is Jan. 31, 2014 through Jan. 31, 2015.
1. CMS has stated that Section IV, Subsection (b) of the Qualified Health Plan Certification Agreement and Privacy and Security Agreement between Qualified Health Plan Issuer and the Centers for Medicare & Medicaid Services (the Subsection) was inserted “at the request of issuers," and that both parties believe the clause is critical. Why is the clause critical?
2. Provide all documents and communication regarding the Subsection. This production should include, but is not limited to, all documents and communication regarding:
a. The purpose of, need for, or language of the subsection; and
b. Requests for a new termination clause, or the risks or likelihood of APTCs ceasing to be available, by a Qualified Health Plan subject to the agreement.
Source: Ranking Member’s News