WASHINGTON - Ways and Means Ranking Member Sander Levin (D-MI) and Energy and Commerce Ranking Member Henry A. Waxman (D-CA) today released a Government Accountability Office (GAO) report revealing that the Medicare Trust Fund could save billions of dollars if the Centers for Medicare and Medicaid Services (CMS) adjusts payments for Medicare Advantage (MA) plans to more accurately reflect the health of MA enrollees.
The GAO report, Medicare Advantage: Substantial Excess Payments Underscore Need for CMS to Improve Accuracy of Risk Score Adjustments, is an update of an earlier report, and finds that the Medicare program continues to overpay MA plans despite CMS' efforts to adjust payments to more accurately reflect the health status of a beneficiary. The report reevaluates the methodology used by CMS to adjust MA risk scores and recommends that the Agency take additional steps to improve the accuracy of these scores. While a more accurate adjustment would increase payments for some beneficiaries, it would decrease payments for others. On net, GAO estimates that the recommended methodological improvements would have saved the Medicare program $3.2 to $5.1 billion in MA plan payments from 2010 to 2012.
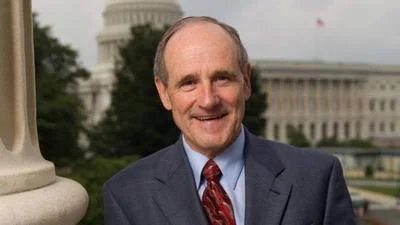
"The Affordable Care Act reined in overpayments to private plans, but this report makes it clear that there is more to be done," said Rep. Levin. "As we continue to look for opportunities to eliminate waste, fraud and abuse in Medicare and pay for physician payment reform, payment accuracy should be one of the first steps we take."
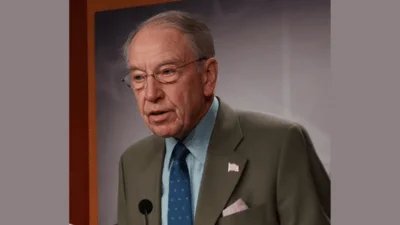
“While CMS has continued to strengthen the Medicare Advantage program, today’s GAO report provides evidence that there is yet more to do," said Rep. Waxman. “One of the best ways to protect Medicare for generations to come is to ensure that the program isn’t overspending for care and services. This GAO report provides Congress with more options for consideration."
The Medicare Advantage (MA) program has grown substantially in recent years, increasing from $65.2 billion in 2006 to $123 billion in 2012. While Congress took action through the Affordable Care Act (ACA) in 2010 to reduce excessive base rate payment rates to private plans, those payments continue to be adjusted to reflect the relative health and risk associated with each beneficiary. However, these adjustments depend on the plans’ own reporting of patient severity.
Documented evidence shows that MA plans tend to report higher patient severity than is actually supported by medical records. It also shows that the reported patient severity increases faster than for comparable patients in traditional fee-for-service Medicare (FFS). In 2005, the Deficit Reduction Act required CMS to reflect differences in coding patterns between MA plans and FFS in its risk score calculations for three years beginning in 2008, to the extent that the impact of such differences on risk scores could be identified. CMS did not adjust risk scores in 2008 or 2009; however, it did estimate and implement a 3.41% reduction in risk scores in 2010.
The ACA required CMS to continue adjusting risk scores for coding differences until CMS implements risk adjustment using encounter data from MA plans. In response, CMS reduced MA beneficiary risk scores by 3.41% in each of years 2010 through 2013. In addition, the ACA required CMS to reduce MA risk scores by at least 1.3% more than the 2010 adjustment (a total of 4.71%) in 2014 and specified that the annual minimum percentage risk score reduction gradually increase to not less than 5.70% in 2019 and subsequent years. The American Taxpayer Relief Act modified this provision such that the 2014 adjustment must be at least 1.5 percent more than the 2013 level (a total of 4.91%) and specifies that the annual minimum percentage risk score reduction gradually increase to not less than 5.9% in 2019 and subsequent years. GAO’s findings indicate that an adjustment of up to 6.4% is warranted. Doing so would yield billions in future savings, which would help extend Medicare solvency and restrain Part B premium growth.