Like most other careers, the practice of medicine faces shifting cultural norms and debates over merit, equity, and institutional trust.
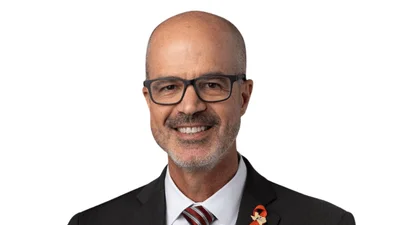
Dr. Leslie Knight’s career cuts through the confusion. A retired Air Force colonel and practicing physician, she built her career on a lifetime of service, skill, and mentorship in the demanding world of military medicine. Her journey offers a case study in how meritocracy can still thrive. Her perspective reveals why earned authority still matters.
Over a 32-year military career, Knight commanded squadrons, flew hundreds of hours as a senior flight surgeon, and earned accolades, including the Legion of Merit and the Bronze Star. Today, she works in a telehealth practice and is involved in professional development initiatives.
Knight’s decision to enter medicine—and military medicine—was shaped by both circumstance and a sense of purpose. Growing up in Maryland with a father who was a state trooper, she was accustomed to a structured lifestyle. “I didn’t know what I wanted to do,” Knight says. Initially considering nursing, she pivoted after seeing her dormmates’ grueling workload and care plans. “I read the care plans…I don’t care about any of that stuff.” she says. I wanted to get my terminal degree, so I said, ‘I’ll just go to med school.’”
She found her path at the Uniformed Services University, a choice prompted by a Parade magazine article her father showed her about a military medical school that paid for tuition in exchange for service. “It was actually the only school I got into,” Knight says. “God had a plan.”
Her choice to specialize in family medicine came from her love of variety and connection. “I loved delivering babies, I loved kids, I loved old people,” she says, and adds, “I thought if I’m a surgeon, I’ll never get to deliver another baby.” Despite a grueling rotation at Fort Gordon, Georgia, Knight pursued family medicine with an OB concentration, finding a calling that allowed her to serve diverse patients throughout their lives.
Knight's experiences in the military highlighted the challenges and the strengths of the system. “I felt like [the military] was a meritocracy,” she says, although she acknowledges where that view was not always accurate. “There was some disrespect here and there.”
Still, she believes the Air Force made serious efforts to ensure fairness, including discouraging pronouns in officer performance reports to minimize unconscious bias during promotion evaluations. “I made it a point not to look at the name when I was scoring a record,” Knight says. “I knew that there is such a thing as unconscious bias and I didn’t want it to affect me.”
Throughout her career, mentorship and sponsorship became central to her leadership style. “Mentoring is really a relationship where people come to you for advice,” compared to sponsorship, which she describes as “when you take someone under your wing and put them forward for opportunities.” She credits mentorship with helping her navigate the male-dominated world of military medicine and emphasizes its critical role in professional development.
Recognizing the need for more targeted support, Knight helped establish the Council for Female Physician Recruitment and Retention. “We found out that the most common point for female physicians to separate was at the level of major or O-4, which is the prime of a career,” she notes. Through initiatives like a female physician leadership course, they worked to increase retention by teaching women how to find mentors, take leadership roles, and confidently navigate military culture.
Knight sees gender diversity as crucial for better outcomes. “Studies have shown that when a team becomes 30% female, they have better outcomes,” she says. Having different experiences and perspectives in the room leads to stronger decision-making and innovation. “If we’re all saying the same thing, one of us is not needed—and it’s probably not me,” she says.
While she praises the military’s historic commitment to meritocracy, Knight is candid about the tensions in today’s culture wars. She supports maintaining merit-based standards but warns against discarding valuable programs under the banner of fighting “wokeness.” She cites the insider threat training mandated after Jan. 6 as an example of a shift that made her feel alienated from the institution she served for decades. “I clearly remember having to do four hours of training telling me that me and the way I thought were the threat,” she says. Disillusioned, she decided it was time to retire.
Now practicing telehealth, Knight continues to adapt to the evolving landscape of medicine. “People want health care that is convenient, affordable, and easily accessible,” she says. New technology allows her to perform heart and lung exams remotely with patient-provided devices. However, Knight stresses that while telehealth can extend access, it cannot replace the depth of training required for full medical practice.
“Physicians are the most highly trained members of the medical team,” she says, noting that even family medicine physicians have over 15,000 hours of training compared to the 800 hours many nurse practitioners graduate with.
Knight also expresses concern about the looming shortage of primary care physicians, calling for more government investment in residency programs. “If we want a healthy population, we need more internal medicine, family medicine, and pediatrics,” she says.