Dear Acting Administrator Norwalk:
The Committee on Finance has exclusive jurisdiction over the Medicare program in the Senate, and the Committee on Ways and Means has jurisdiction over the Medicare program in the House of Representatives. Accordingly, we have a responsibility to the more than 40 million Americans who receive health care under the program. We take this responsibility seriously and conduct oversight into the activities of executive branch agencies, including the Centers for Medicare and Medicaid Services (CMS), to ensure that program dollars are spent on the best care available to beneficiaries.
The Medicare and Medicaid programs spend in excess of $120 billion for inpatient healthcare services at thousands of American hospitals annually-including payments made to physician-owned specialty hospitals. For years, we have been outspoken critics of the conflicts created by physician-owned specialty hospitals.
Together, we have held hearings, conducted oversight, commissioned studies, and even passed legislation regarding these facilities. We write today to renew our concerns and to inquire about yet another disturbing patient death at a physician-owned specialty hospital.
As you are aware, the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) imposed an 18-month moratorium on Medicare payments to new physician-owned specialty hospitals. The statutory moratorium expired in June 2005. Through administrative action, CMS began a suspension on enrollment of new facilities from June 2005 through August 2006, when CMS released the final Strategic and Implementing Plan for Specialty Hospitals that was mandated by the Deficit Reduction Act of 2005 (DRA). The difference between the statutory moratorium and the administrative suspension on enrollment took center stage at a Finance Committee hearing held May 17, 2006.
The May 2006 Finance Committee hearing focused on the death of a patient at a physician-owned surgical hospital in Oregon that had opened for business during the MMA moratorium. The tragic death at the Oregon facility was even more egregious because the staff at the physician-owned hospital called 911 for an ambulance to transport the patient from the physician-owned hospital to a community hospital with an emergency room. We remain dismayed that a physician-owned hospital’s standing policy in treating a patient in an emergency situation is to call 911.
We are even more troubled today, after learning of this same scenario playing out again at another physician-owned specialty hospital-this time in Texas. It has been reported that on Jan. 23, 2007, staff at West Texas Hospital-a physician-owned specialty hospital-placed an emergency call to 911 after a patient went into respiratory arrest several hours following an elective spinal surgery. Following the emergency call,
the patient was transferred to a community hospital, Abilene Regional Medical Center,
where he later passed away.
We are deeply disturbed by these events and want to find out more about what transpired. It is utterly unacceptable to us that we now have witnessed two separate incidents where patients were treated at “hospitals" that maintained a policy of calling
911 for emergency resuscitation of a patient following major elective surgery. CMS clearly must take action and ensure that physician-owned facilities that hold themselves out to the public as “hospitals" have the requisite staff and abilities to ensure that basic lifesaving measures can be employed.
From a review of previous records requests made by the Finance Committee to CMS regarding physician-owned specialty hospitals, it appears that West Texas Hospital was granted its Medicare provider number on May 20, 2005, making it another physician-owned facility granted a Medicare provider number during the MMA moratorium. Further, these records show that West Texas Hospital has been reimbursed
$4,193,702 by Medicare since it was granted its Medicare provider number in 2005.
While we recognize it is CMS’s position that the granting of a provider number during the moratorium was acceptable, CMS has stated that any Medicare payments made to hospitals during the moratorium are subject to review and possible recovery by CMS.
We are concerned with the fact that West Texas Hospital appears to have opened during the moratorium and that it appears to have received Medicare funding for procedures performed during this timeframe.. Accordingly, we request detailed written responses to the following:
(1) Why did West Texas Hospital receive a Medicare provider number from CMS during the MMA mandated moratorium on physician-owned specialty hospitals?
a. Did West Texas Hospital file a request for an advisory opinion to determine if it qualified for the “under development" exception to the MMA moratorium? If so, please provide any documentation.
b. Please describe in detail the events surrounding the application for and granting of a Medicare provider number for West Texas Hospital.
(2) Provide a list of all Medicare and Medicaid reimbursements paid to West Texas Hospital or any provider affiliated with West Texas Hospital from 2005 to the present.
a. Were any of the Medicare payments made during the statutorily mandated moratorium on payments?
b. If so, has CMS initiated any action to collect the payments made during this period? If not, why?
(3) Provide a list of all physician owners of West Texas Hospital?
(4) Has CMS conducted any surveys of West Texas Hospital? If so, provide a copy of all such surveys.
(5) Did West Texas Hospital provide responses to CMS’s survey on physician owned specialty hospitals that was sent in an effort to collect information for the Strategic and Implementing Plan for Specialty Hospitals? If so, please provide a copy of West Texas Hospital’s responses.
(6) Does West Texas Hospital provide notification to patients prior to surgery that in the event of an emergency, they may be transferred to another hospital and that the facility may not have a physician on site during the post-operative recovery period?
(7) How many times in the past has West Texas Hospital called 911 to transfer a patient to another hospital in an emergency situation?
We thank you in advance for your cooperation and request that your staff provide a point of contact for this matter no later than Feb. 12, 2007. Additionally, we request that CMS provide a briefing on this matter as soon as all written responses are available, not later than Feb. 21, 2007. In complying with this request for information, please respond to each enumerated question by repeating the questions,
followed by CMS’s response.
Should you have any questions regarding this matter please contact David Schwartz or Billy Wynne of Senator Baucus’ staff or Michael Park or Nick Podsiadly of Senator Grassley’s staff at (202) 224-4515 or Debbie Curtis of Representative Stark’s staff at (202) 225-5065.
Sincerely,
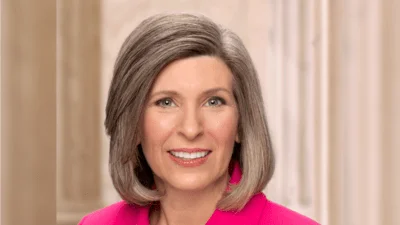
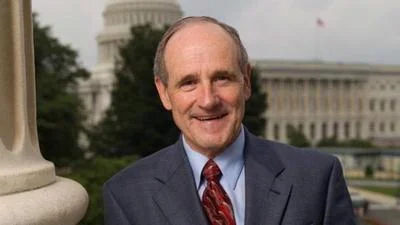
Max Baucus, Chairman, Senate Committee on Finance Charles E. Grassley, Ranking Member, Senate Committee on Finance Pete Stark, Chairman, Subcommittee on Health,
House Committee on Ways and Means
Cc: Dr. David L. Lakey, Commissioner Texas Department of State Health Services West Texas Hospital
5602 Health Center Drive Abilene, Texas 79606
Source: Ranking Member’s News