Dear Mr. Rand:
I appreciate AARP’s continued cooperation with my staff and with the United States Senate Committee on Finance (“Committee") regarding AARP-licensed health insurance policies. The briefings, responses, and document productions provided have helped my staff shed light on AARP-licensed supplemental indemnity plans such as the “Essential Plus Health Insurance Plan" (EPHIP) and the “Essential Health Insurance Plan" (EHIP). I want to take this opportunity to share with you my findings, recommendations, and additional requests regarding my inquiry.
Last year, I initiated this inquiry following Committee testimony by Lisa Kelly, a cancer patient treated at M.D. Anderson Cancer Center in Houston, Texas. Allegedly led to believe she had purchased AARP-licensed health insurance, Ms. Kelly found herself asked to pay tens of thousands of dollars before she would be treated because of the very limited nature of her AARP-licensed supplemental indemnity plan (“indemnity plans" or “limited benefit policy"). I have also been made aware of the case of Janice and Gary Clausen, of Audubon, Iowa.
Apparently misled about the potential cost of medical care and the adequacy of limited benefit plans, the Clausens purchased an AARP-licensed limited benefit plan for about $500 per month.
Soon after, Gary Clausen was diagnosed with colon cancer and the family was left with over
$150,000 in medical debt. The claims that Ms. Kelly and the Clausens had been mislead in their search for health insurance resulted in my staff reviewing AARP’s marketing materials and to my subsequent launch of this inquiry.
A preliminary review of AARP’s written and online marketing materials suggest that these indemnity plans are neither health insurance in fact nor an adequate alternative. An AARP brochure on the indemnity plans describes them as a “smart option for the health care insurance you need," then, in smaller font, “an indemnity plan that pays you fixed cash benefits for covered doctor’s appointments, prescriptions, hospital stays, surgeries, outpatient lab tests, emergency room visits and more - even though it’s not a major medical plan." The promotional website goes on to instruct individuals to apply for MAP if they “don’t have health coverage," need “a
‘bridge’ to Medicare or until other coverage is available," or “need to lower [their] medical expenses." Another promotional document, titled “Let me tell you how your plan works!"
describes how the plan pays for procedures. The document lists only a limited sample of lowercost procedures such as an outpatient diagnostic colonoscopy. The document offers no examples of how the benefit works for a surgery other than the relatively lower cost procedure, diagnostic colonoscopy, which is not typically referred to as surgery. Moreover, the AARP document provides no example of how the benefit would apply to an inpatient hospital stay or a surgery of average cost. Telephone calls placed to AARP telephone sales representatives by my staff raised further concerns about the information disclosed, or not disclosed, to AARP members seeking health insurance.
Following this review, Committee staff held a preliminary meeting with AARP officials to discuss the indemnity plans. During the meeting, these representatives stated that indemnity plans, like the one purchased by Lisa Kelly for nearly $200 per month, were designed to be purchased in addition to other health insurance, but for someone with no coverage, the plans were, at least, “better than nothing." They went on to say that they believed that these fixed indemnity plans, which are targeted to people between 50 and 65 years of age, are indeed purchased mostly by those who have no other health insurance. These differences in policy design, AARP’s marketing campaign, and the acknowledged reality of the indemnity plan market led me to launch a more in-depth inquiry into this matter.
On Nov. 3, 2008, I wrote AARP a letter outlining the issues raised above and subsequent concerns identified by Committee staff, as well as raising a number of additional questions. This letter requested information regarding AARP’s marketing materials, telephone representative talking points, what policies or programs the indemnity plans were designed to
“bridge," complaints received, and other matters. I am attaching a copy of that letter for your convenience. Let me also take this opportunity to outline the information provided in response to this request.
AARP licenses its name to UnitedHealth Group (“United,") which is the carrier for the indemnity plans in question. United is responsible for the marketing, sales, and administration of these policies; although AARP Services, Inc. oversees and monitors all use of AARP’s name,
approves all marketing materials, and monitors certain call-center activities. Calls to AARP regarding the indemnity plans are often answered and serviced by Catalyst360, a division of Hartford Fire Insurance Company.
Regarding the marketing of these indemnity plans, AARP stated that United widely advertises the plans without regard to current coverage or health status. While United focuses advertising activities on AARP members between 50 and 64, they do so with no knowledge of the member’s current insurance status. Despite this, AARP stated that these indemnity plans are designed to “provide a supplemental coverage option to AARP members who already have comprehensive coverage but want to supplement their coverage." Despite this design, AARP call center representatives are instructed to tell AARP members with no other insurance “the importance of having sufficient health insurance to help with medical expenses and how [AARPlicensed indemnity plans are] uniquely designed as an affordable alternative to expensive major medical insurance," (emphasis added.) The indemnity plans, according to the AARP materials,
“may also be the only option available to individuals who do not qualify for, or cannot afford,
comprehensive insurance."
This leaves open the question of whether AARP members that do not qualify for or can’t afford “comprehensive insurance" are expressly advised of the limited nature of the plans they are purchasing. For these members, call center employees are instructed to proceed in a way that
“assesses the caller’s eligibility and reviews the indemnity... products with the caller." AARP’s response makes clear that these AARP members are then directed toward only an AARPlicensed product and not non-AARP policies available that may better cover the AARP member.
When talking to AARP members who cannot afford more comprehensive AARP-licensed policies, call center employees describe the indemnity plans as an “affordable alternative to major medical" and an “excellent choice" to an individual seeking a “less expensive option" to major medical insurance. Call center employees are also instructed specifically not to mention preexisting condition exclusions unless they are explicitly asked about them by members.
AARP marketing materials state that these indemnity plans are for individuals needing “a
‘bridge’ to Medicare or until other coverage is available." Asked for further explanation of this statement, AARP stated that the indemnity plans help AARP members bridge a “limited" period of time, such as when they would otherwise go uninsured for financial or underwriting reasons including being between jobs, not yet being eligible for employer-sponsored coverage, in retirement but not yet Medicare eligible, or in cases that they otherwise cannot afford or qualify for comprehensive health insurance. In light of AARP’s statement that these plans were designed to supplement, rather than supplant, comprehensive health insurance, this makes the sufficiency of AARP’s marketing materials all the more crucial. AARP’s response again made clear that, in cases of AARP members needing this “bridge," AARP markets to those individuals only AARP-licensed products that are available to them.
My letter of Nov. 3, 2008 also requested information regarding complaints and other communications AARP received concerning their indemnity plans. AARP explained that complaints and communications regarding these indemnity plans are received by AARP, United,
and Catalyst360. These complaints and communications aren’t categorized specifically as complaints or concerns, and are not maintained in a consistent manner by the three entities. As a result of not maintaining complaint information in a consistent and centralized manner across the three entities that monitor complaints, AARP can neither adequately identify nor evaluate the concerns and complaints lodged by its members who purchased an AARP-licensed indemnity plan.
Again, the briefings, responses, and document productions provided by AARP have been very helpful in assisting my Committee staff review this matter. After reviewing these materials and Committee staff findings, I want to take this opportunity to share with you additional recommendations and requests regarding my inquiry.
While AARP-licensed indemnity plans are marketed without regard to a member’s insurance status, your organization’s marketing materials make clear that the uninsured are a sought after customer and marketing techniques were designed to sell them indemnity plans without regard to better options found elsewhere in the market. These materials establish that AARP actively markets fixed-benefit indemnity plans to AARP members without medical insurance. The marketing materials accomplish this by highlighting certain low-cost medical procedures that are typically reimbursed by the indemnity plans. On the other hand the marketing material fails to adequately highlight the risks associated with fixed-benefit indemnity plans. As a result AARP is systematically misleading its members by failing to ensure that they are fully apprised of the risks of underinsurance associated with the indemnity plans that are being sold under its name. Furthermore, by informing its members only of the “best AARP-branded product available," and not non-AARP options that might be, in fact, better for their needs, your organization is in fact doing its members a disservice by failing to present a full menu of the available policies that may better suit their needs.
I remain deeply troubled by AARP’s practices regarding its indemnity plans. Further,
these plans have been sold to hundreds of thousands of AARP members, some of whom may reasonably believe they were purchasing health insurance. Having sold these policies to so many AARP members, AARP is also failing to maintain adequate communication systems to monitor its members’ experiences and potential complaints about the product they have been sold under its name. This situation in turn raises the additional question of how individuals currently holding these limited indemnity policies will be advised of their insurance status, how problems they encounter will be monitored and addressed, and how AARP will make things right for those members that were led to believe they were purchasing adequate health insurance.
I request that AARP fully inform those individuals currently holding limited benefit policies about the limited nature of these policies, and provide them with examples of how the policies would work in reality. For these policies and all other AARP-licensed insurance products, AARP should design a system to monitor and categorize complaints and other communications from policyholders to make certain that AARP can adequately monitor its members’ experiences and react responsibly to complaints.
Going forward, I request that AARP provide me with an update on these matters every six months for the remainder of this Congress. The information provided in these updates should include:
1) How AARP’s complaint monitoring system has been improved, the number and nature of complaints received regarding the remaining indemnity plans, and how they were addressed.
2) Any update or modification of AARP’s marketing materials regarding health insurance products it sells, including comparisons to prior versions.
3) Detailed information regarding any information provided to AARP members with existing indemnity plans.
4) The number of AARP policy holders who cancel, switch, or otherwise modify their plans after they receive such information, including how these cancellations and other modifications compare to past activity.
5) Information regarding any civil settlement AARP executes with individuals who hold or held the indemnity plans subject to this inquiry, with names and settlement details omitted.
6) Any actions AARP takes to compensate individuals who purchased an AARP limited benefit policy.
As Congress moves to reform America’s health care system, it is my hope that we can make limited benefit indemnity plans obsolete by making meaningful insurance coverage available to everyone. In the meantime, it is crucial that we make certain that those with existing policies fully and promptly understand them and that those choosing health care coverage can make informed decisions based on accurate, timely and realistic information. Thank you again for your continued cooperation in this matter.
Sincerely,
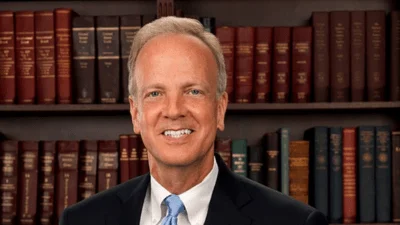
Charles E. Grassley Ranking Member