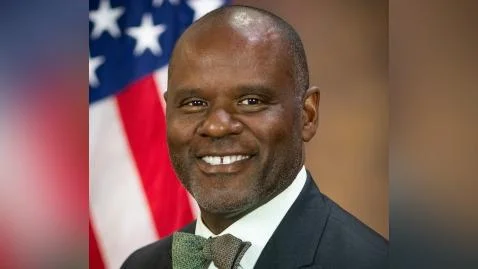
Ismail J. Ramsey, U.S. Attorney | U.S. Attorney for the Northern District of California
American Psychiatric Centers, Inc., which operates as Comprehensive Psychiatric Services (CPS), has agreed to pay $2.75 million to settle allegations that it submitted false claims for psychotherapy services to government healthcare programs. The settlement addresses claims made from January 1, 2015, through December 31, 2022.
CPS is based in Walnut Creek, California and provides behavioral medicine services throughout the state. According to federal authorities, CPS and its providers billed government payors using specific “add-on” codes meant for psychotherapy performed alongside evaluation and management visits. These codes require particular documentation.
Authorities allege that CPS used these codes in situations where the required services were not provided or not properly documented. Of the total settlement amount, $2,615,569.32 will go to the United States and $134,430.68 will be paid to the State of California.
“Providers that participate in federally funded health care programs must abide by the rules and submit proper claims for care that was in fact rendered. To do otherwise is to drain resources from our fellow Americans who rely on Medicare and other government programs. This settlement sends a clear message that we will continue to investigate and pursue any entity that fraudulently seeks to increase profits at taxpayers’ expense,” said United States Attorney Craig H. Missakian.
“Holding health care providers accountable for submitting false claims to Federal health care programs is crucial for ensuring that taxpayer funds are appropriately used and for maintaining the American public’s trust,” said Acting Special Agent in Charge Jeffrey McIntosh of the Department of Health and Human Services Office of Inspector General (HHS-OIG). “Working closely with our law enforcement partners, our agency remains dedicated to protecting taxpayer-funded programs that deliver essential behavioral health services.”
“Today’s outcome concludes a collaborative effort to hold Comprehensive Psychiatric Services accountable for its improper billing practices. These actions undermined our Federal health care system, including the Department of Defense’s TRICARE program,” said John E. Helsing, Acting Special Agent in Charge for the Department of Defense Office of Inspector General, Defense Criminal Investigative Service (DCIS), Western Field Office. “DCIS will continue to work closely with our law enforcement partners and the Department of Justice to investigate health care providers that seek to enrich themselves at the expense of the American taxpayer.”
“Veterans and their families expect and deserve the highest quality healthcare delivered in a safe and accountable setting,” said Special Agent in Charge Dimitriana Nikolov with the Department of Veterans Affairs Office of Inspector General’s Northwest Field Office. “This settlement is a testament to the VA OIG’s commitment to safeguarding the integrity of VA’s healthcare programs and preserving taxpayer funds.”
“False claims increase costs and undermine the integrity of our federal health care programs, including the Federal Employees Health Benefits Program,” said Derek M. Holt, Special Agent in Charge, the U.S. Office of Personnel Management Office of the Inspector General (OPM OIG). “We support the work of our law enforcement partners and colleagues to investigate fraudulent medical billing that wastes taxpayer dollars.”
The matter was handled by Assistant U.S. Attorney Kelsey Helland with assistance from Garland He. Multiple agencies contributed to investigating this case: The U.S. Attorney’s Office for the Northern District of California; HHS-OIG; DCIS; VA OIG; OPM OIG; and California's Division of Medi-Cal Fraud and Elder Abuse.
Federal officials note that combating healthcare fraud remains a priority, with tools such as the False Claims Act being central efforts against wasteful or abusive billing practices.
Authorities emphasized that all resolved claims are allegations only; there has been no finding or admission of liability.