The United States has filed a lawsuit against the Local Initiative Health Authority for Inland Empire Health Plan, known as Inland Empire Health Plan (IEHP), alleging violations of the False Claims Act. IEHP is based in Rancho Cucamonga and operates as a California Local Initiative Health Plan.
IEHP had an agreement with California’s Department of Health Care Services (DHCS) to provide health care services to residents of Riverside County and San Bernardino County through Medi-Cal, the state’s Medicaid program. The government alleges that IEHP made false statements to Medi-Cal and knowingly kept overpayments.
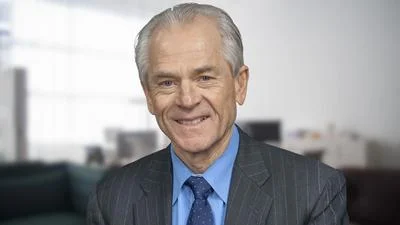
“Today’s lawsuit against IEHP shows our steadfast commitment to hold accountable insurers that brazenly compromise the Medicaid system,” said Acting United States Attorney Bill Essayli. “We will take every measure to restore integrity and accountability to the Medicaid system and ensure that patient care – not financial gain – is the primary focus of our health care system.”
“The Medicaid program provides critical health care services,” said Deputy Assistant Attorney General Brenna Jenny of the Justice Department’s Civil Division. “Today’s complaint demonstrates our continued commitment to protect the integrity of the Medicaid program, and the taxpayer dollars that support it, from health insurers that knowingly seek to divert program funds for their own financial benefit.”
In January 2014, Medi-Cal expanded coverage for adults aged 19-64 without dependent children whose incomes were up to 133% of the federal poverty level. For three years, this expansion was fully funded by the federal government. Under its contract with DHCS, IEHP received funding for this population but was required to spend at least 85% on allowed medical expenses or return any surplus above this threshold. California would then return these funds to the federal government.
According to court documents, IEHP allegedly created schemes involving sham incentive programs and a retroactive rate increase outside its contract terms. These actions reportedly led IEHP to use surplus Medi-Cal Expansion funds improperly, such as covering administrative costs or benefiting other patient groups rather than spending on permitted medical expenses.
The complaint further states that IEHP disguised payments for consultants and technology services as incentive payments by routing them through providers and backdating expenditures. Internal communications at IEHP reportedly acknowledged giving providers “free money,” while externally describing these as performance-based incentives.
The case is being managed by attorneys from both the Civil Division’s Commercial Litigation Branch Fraud Section and the U.S. Attorney’s Office for the Central District of California, working alongside state agencies including HHS-OIG and DHCS.
The claims in this lawsuit are allegations only; there has been no finding of liability at this stage.