The U.S. Department of Labor (DOL) recently issued a temporary enforcement policy for brokers and consultants of Employee Retirement Income Security Act (ERISA) health plans, requiring them to disclose their compensation to clients.
Field Assistance Bulletin 2021-03, released by DOL’s Employee Benefits Security Administration on Dec. 30, 2021, is a soft launch for the new ERISA rule requiring insurance providers to disclose “detailed information to plan fiduciaries about the compensation that providers expect to be paid in connection with their services to the plan,” a DOL press release said.
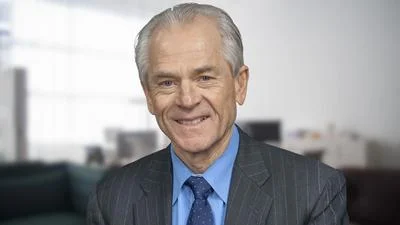
“The new disclosure requirements will help group health plans and their fiduciaries by shedding needed light on some of the complex and often opaque fee-sharing arrangements that unfortunately typify aspects of our healthcare system,” Acting Assistant Secretary of Labor for Employee Benefits Security Ali Khawar said in the release.
While the amendment will be enforced, the bulletin allows conditional relief to those who fail to meet the new requirements but work in good faith to do so and have a reasonable interpretation of the rule, Bulletin 2021-03 said.
“The Field Assistance Bulletin gives plans and their brokerage and consulting service providers some transitional flexibility as they build systems to implement the new disclosure requirements, but that flexibility depends on reasonable and good faith behavior,” Khawar said in the release.
The bulletin also contains a question and answer section to help explain the requirement in respect to several key issues.
“The Consolidated Appropriations Act, 2021 included amendments of prohibited transaction exemption provisions in ERISA section 408(b)(2) that govern service provider arrangements with ERISA plans,” the release said. “Both the pension and group health plan disclosure provisions specifically focus on helping plan fiduciaries guard against conflicts of interest that may arise when plan service providers receive compensation from third-parties.”