Dear Secretary Leavitt:
The United States Senate Committee on Finance (Committee) has exclusive jurisdiction over, among other things, the Medicare and Medicaid programs. As Chairman and Ranking Member of the Committee, we have a responsibility to protect these programs along with the more than 80 million Americans who receive healthcare from them.
Each year the Medicare and Medicaid programs spend in excess of $200 billion for in-patient healthcare services at America’s hospitals. Managed by the Centers for Medicare and Medicaid Services (CMS), Medicare and Medicaid cover many different procedures and services reaching virtually every hospital across the country, including physician-owned specialty hospitals. These physician-owned specialty hospitals have raised much controversy and debate over the past few years. Concerns over their dramatic growth, among other things, led Congress to enact section 507 of the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MMA) -- an 18-
month moratorium on the construction of new physician-owned specialty hospitals. We write today to express serious concerns about both CMS’ administration of the specialty hospital moratorium and the quality of care and patient safety at physician-owned specialty hospitals.
Physicians’ Hospital (Physicians’) in Portland, Oregon, is in many ways the typical specialty hospital. Physicians’ focuses primarily on orthopedic and neurosurgical procedures and the primary investors are doctors who work at the hospital. However, Physicians’ differs from other specialty hospitals in that it appears to have opened its doors for business in December of 2004, during the 18-
month moratorium Congress placed on specialty hospitals. This information was brought to our attention as a result of a tragic event which occurred this past summer at Physicians’.
The Case of Helen Wilson:
On July 27, 2005, Helen Wilson, an 88-year-old woman with a history of hypertension and diabetes,
was admitted to Physicians’ for elective back surgery. While in recovery, Ms. Wilson was given an injection of the pain medication hydromorphone, and suddenly went into cardiac arrest. The nursing staff at Physicians’ immediately began CPR, but there was no doctor available to assist. According to the investigative report filed by the Health Care Licensure and Certification Office of the Oregon Department of Human Services,
“[T]here was no physician in the hospital at the time of the incident. The hospital does not have an emergency department. The respiratory therapists are not permitted to intubate patients. The hospital’s [Physicians’] policy is to call 911 in the event of a patient code."
The nurses followed procedure and called 911 for emergency help. Upon arriving at Physicians’,
paramedics were able to intubate and resuscitate Ms. Wilson and transport her to a neighboring hospital capable of providing a higher level of care. Unfortunately, it was too late. Ms. Wilson passed away four days later, after her family made the decision to remove life support.
The investigative report indicated that a review of documentation and interviews with hospital staff revealed that “the hospital failed to ensure that the medical staff was accountable for the quality of care provided to all patients." The report raises questions regarding whether the admitting physician actually assessed the patient prior to surgery, whether the surgery was still necessary, and whether it was appropriate given the patient’s abnormal laboratory values prior to surgery. The report also finds that a nurse made “multiple unsuccessful calls to several physicians between the hours of 1655 and 1720," just before the patient stopped breathing.
The events surrounding the death of Helen Wilson are tragic, and illustrate some of the drawbacks of the limited scope of work performed at specialty hospitals. This incident raises concerns about quality of care and patient safety. Additionally, it raises questions regarding how Physicians’ was allowed to open during the 18-month MMA-mandated moratorium.
Specialty Hospital Moratorium:
Physicians’ Hospital, a physician-owned orthopedic and neurosurgical specialty hospital, opened for business in December 2004, in the middle of the 18-month moratorium. Further, initial inquiries to CMS by our staff revealed that Physicians’ Hospital did not request an advisory opinion to determine whether the facility qualified for an exception available to certain specialty hospitals under development. (End Note 1) Thus, we are left in the position of wondering how Physicians’ was able to open its doors for business during the specialty hospital moratorium.
Based upon our review of information provided by CMS, even if Physicians’ did apply for an advisory opinion it should not have qualified because the official transaction to purchase Physicians’
did not occur until July of 2004, well after the Nov. 18, 2003, deadline imposed by CMS.
Perhaps an alternative explanation is that Physicians’ operated using the provider number of the previous hospital run at the same location, Woodland Park Hospital, a full-service community hospital. In either case, it appears that CMS should not have allowed Medicare or Medicaid payments to Physicians’. Accordingly, as Chairman and Ranking Member of the Committee, we request that you provide written responses to the following:
(1) How many physician-owned specialty hospitals have policies, either written or verbal, that do not require a physician to be on duty or on call when patients are present?
a. Do any of these physician-owned specialty hospitals provide a disclaimer to their patients informing them that a doctor may not be there in the event of a life-threatening emergency?
b. In the event that CMS does not track or have records that would allow CMS to answer the aforementioned questions, please provide a written response regarding CMS’ position as to whether or not CMS believes Medicare and Medicaid funds should be paid to specialty hospitals that lack either a physician on duty or a physician on call.
(2) How many physician-owned specialty hospitals have policies directing hospital staff to call 911 in case of a patient emergency?
(3) Since its opening in December 2004, have there been any other patient deaths at Physicians’?
What are the circumstances surrounding these deaths?
(4) Was Physicians’ Hospital reimbursed by Medicare or Medicaid for any services rendered during or after the physician-owned specialty hospital moratorium (Nov. 18, 2003 - Present)? If so,
please provide a list of the payments, including the type of procedure and the total amount of money reimbursed.
(5) Was Physicians’ granted a new provider agreement to receive Medicare and Medicaid payments?
a. If so, please provide an explanation why CMS issued a provider agreement to a new physicianowned specialty hospital during the moratorium.
b. If not, please state in detail how Physicians’ was able to seek reimbursement for services to Medicare and Medicaid patients.
(6) Is CMS aware of any other physician-owned specialty hospitals that have received provider agreements during the moratorium without applying for the required advisory opinion? If so, please provide a list of the hospitals and a reason why CMS granted a provider agreement.
(7) Does CMS know of any other physician-owned specialty hospitals similar to Physicians’ that may have opened during the moratorium utilizing a provider agreement from a facility that existed prior to the moratorium? If so, please provide a list of such facilities and provide a detailed explanation as to why CMS approved them during the moratorium.
(8) Provide a list of all specialty hospitals that received any payment from Medicare and Medicaid from Nov. 18, 2003, through June 8, 2005. This list should include the name of the facility, the location, and contact information for that facility. Please separate this list by state and identify the total amount of Medicare and Medicaid funds received by each facility.
The case of Helen Wilson raises overall patient health and safety concerns of physician-owned specialty hospitals. The public expects any facility labeled as a “hospital" to be able to appropriately deal with urgent medical situations. This involves more than just dialing 911 and waiting for an ambulance to arrive. Medicare beneficiaries should receive care in hospitals that are adequately staffed to deal with complications that may arise before, during, or after surgical procedures performed at the hospital.
If it is determined that Physicians’ was given a new provider agreement during the 18-month moratorium, it raises serious questions about the number of these facilities operating across the country and the integrity of CMS’ enforcement of the moratorium. Conversely, if this facility acted based upon the provider agreement from its predecessor, Woodland Park Hospital, it raises questions regarding the accuracy of CMS’ records and CMS’ ability to track new hospitals. At best, it is safe to say that the circumstances surrounding Physicians’ and its receipt of Medicare and Medicaid funds are unclear.
We thank you in advance for your cooperation and request that your staff provide a point of contact for this matter no later than Feb. 17, 2005. Additionally, we request that CMS provide a briefing on this matter as soon as all written responses are available, not later than Feb. 28, 2005. In complying with this request for information, please respond to each enumerated question by repeating the questions, followed by CMS’ response.
Sincerely,
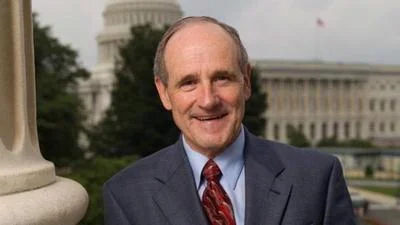
Charles E. Grassley
Chairman
Max Baucus Ranking Member
Cc: The Honorable Mark McClellan, M.D., Ph.D.
(1) See 42 U.S.C. § 1395nn(h)(7)(B)(i) (2006).
-30-
Source: Ranking Member’s News