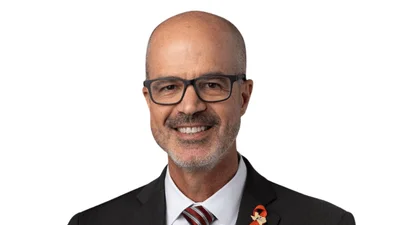
Kirsten Axelsen has worked in the biopharmaceutical industry for 24 years and is a nonresident fellow at the American Enterprise Institute.
This transcript has been edited for length and clarity.
Federal Newswire: What is your view of the pharmaceutical industry?
Axelsen: I believe that competitive forces and market-based incentives are the right way to encourage development and transformational cures. There are flaws in the system, but I would rather see the epidemiology of disease and the private market driving where investment goes and what diseases are studied rather than political or emotional decisions.
Federal Newswire: What’s an example of where this is not working?
Axelsen: [There is a federal program] intended to help hospitals that serve disproportionately large numbers of higher-need people. Those hospitals are able to purchase drugs at deeply discounted prices and receive whatever price the beneficiary’s insurance pays them for that drug.
This helps funnel money to the hospitals that are treating high-need people. It is important to get money to hospitals that are treating high-need people. However, any person who understands financial incentives would say, wait a second, that creates an incentive to use the most expensive drugs with the most well-insured people.
What we've seen is a big expansion of hospitals, in particular provider groups who treat oncology patients, purchasing expensive drugs. You can get a very well reimbursed drug and at a very low price. If this money were going back into patient care, or if this money were going to relieve medical debt for low income people, maybe it would be a fine system.
Federal Newswire: Does this create opportunities to cheat the system?
Axelsen: Absolutely. When you think about the incentives, the structure sets up a way for the hospital to maximize the benefit from this program [by going] into higher income neighborhoods and acquiring practices that dispense expensive drugs, [which] increases their use of expensive drugs. It increases consolidation.
There are changes that could be made to the program that would, for example, direct the funds to low income people. But I would argue funding hospitals based on the arbitrage, opportunity, and a drug price is not the right way to do it.
Federal Newswire: Does this impact innovation for pharmaceutical companies?
Axelsen: This is now the second largest program in the United States after Medicare. We know, based on prior studies, that the Medicare program affects the direction of investment in clinical studies.
The program, by reducing the size of the market, does have the potential to reduce investment in clinical study. It also is likely raising the initial price a drug is set at before other discounts are offered. That affects the out-of-pocket costs for people who have co-insurance or people who are not insured. It definitely has a distorting effect on both pricing and clinical development decisions.
Federal Newswire: Is there a way for bio companies to be part of communities as opposed to just big entities that make lots of money?
Axelsen: There is no ‘small pharma’ without ‘big pharma.’ There is no funding for academic centers without the anticipation that some of their programs are going to be profitable.
It's a very high risk business. That means that, like any gamble, you have to do really well sometimes to offset the times that you really don't do well. For us, doing really well means there's a cure for a rare disease.
Federal Newswire: Should the government benefit more from pharmaceutical innovations that it helps fund?
Axelsen: There's a good number of drugs that had federal funding in their clinical development programs early on, often through grants to academic centers. There are very few drugs developed entirely with federal government funding.
“Marching Rights” were put in place to allow others to manufacture a patented drug if a company is not meeting its obligations to supply the necessary amount for a population, [and] if the government has invested in their clinical development program.
Marching Rights have never been exercised, even though the NIH has been asked to exercise them multiple times, because the directors have said there is sufficient supply.
Marching Rights essentially make collaborations with academic centers way riskier, way less valuable. And I would even say toxic at a time when other countries, in particular China, are doing a really good job at building up their capacity to do early R&D. It's not like there aren't other places to go for it. I think it would be a huge threat to not only medical innovation, but to academic centers in many states.