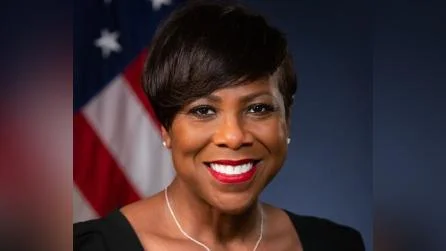
Dawn N. Ison, U.S. Attorney | Department Of Justice Eastern District Of Michigan
United States Attorney Dawn N. Ison announced that Commonwealth Care Alliance, Inc. (CCA) will pay $520,355.65 to settle allegations related to violations of the False Claims Act by Reliance HMO, Inc., a company acquired by CCA in 2022. The accusations involve cash payments made to induce referrals for Medicare beneficiaries into Reliance’s Medicare Advantage Plan, contravening the Anti-Kickback Statute.
Medicare Advantage Plans are managed care insurance plans under the Medicare Part C program, where CMS provides monthly payments for each enrolled beneficiary. The Anti-Kickback Statute prohibits remuneration in exchange for referrals within federal healthcare programs.
CCA is a not-for-profit organization based in Boston offering MA Plans. In April 2019, CMS authorized Reliance HMO to operate an MA plan in Michigan with coverage starting January 2020. After acquiring a majority stake in Reliance on March 31, 2022, CCA identified concerns about certain marketing practices and payments made by Reliance agents.
Two specific schemes were disclosed: first, between April 12, 2019, and December 22, 2020, cash payments were made to healthcare professionals for patient contact information; second, in November 2019, before its MA plan activation, Reliance paid four physicians $2,500 each as advances on "coordination of care" services.
The United States alleges these actions aimed at inducing enrollment recommendations or arrangements constituted illegal kickbacks under the False Claims Act. CCA's voluntary disclosure led to credit being given for cooperation and remedial measures taken included terminating involved employees and providing detailed investigation reports.
U.S. Attorney Ison emphasized the importance of self-disclosure and remedial action: “Our office encourages companies and individuals to make timely self-disclosures and take remedial measures to mitigate the harm from fraud that they discover.” Special Agent Mario Pinto highlighted the role of HHS-OIG’s Self-Disclosure Program: "This settlement highlights the value of HHS-OIG’s Self-Disclosure Program."
The U.S. Attorney’s Office urges reporting any waste or fraud through their hotline or website links provided for self-disclosure protocols.
Assistant U.S. Attorney Jonny Zajac handled this civil investigation with assistance from HHS-OIG.
It is noted that these claims are allegations only without any determination or admission of liability.