As the United States grapples with healthcare costs, an overlooked contributor to costs is coming under scrutiny: nonprofit hospitals. Despite their tax-exempt status, these institutions—comprising 60% of U.S. hospitals—are viewed by some critics as falling short of their charitable obligations, spending less on community care than they receive in public subsidies.
A new report describes a $25.7 billion “fair share deficit” created by the non-profits, and argues that they are misusing taxpayer dollars while avoiding public accountability. With bipartisan reform proposals emerging in Congress and growing momentum at the state level, the debate over nonprofit hospitals is shifting to a call for transparency, oversight, and meaningful structural change.
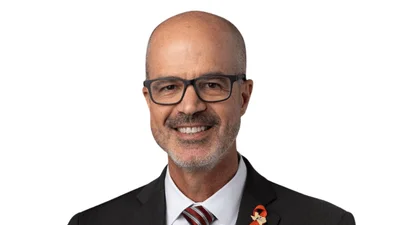
The report is authored by Peter Pitts, president and co-founder of the Center for Medicine in the Public Interest and a former FDA associate commissioner. The report, titled Unmasking the Real Cost Drivers of U.S. Health Care, describes “a shocking level of misappropriation” in the nonprofit hospital sector.
“When you ask most Americans where healthcare dollars go, everybody says, ‘pharmaceuticals,’” Pitts says. “And that’s not true. Drugs are about a dime on the dollar—10% of U.S. healthcare expenses. Hospitals are between 30 and 35%. But nobody talks about that.” Pitts argues that if policymakers want to fix the system, they need to “go where the money is”—and that means hospitals.
According to Pitts, 60% of hospitals in the U.S. are nonprofits, yet “eight out of ten spend less on community or charity care than they receive in tax breaks.” This creates what Pitts calls a “fair share deficit,” which he says totals $25.7 billion nationwide—more than enough to pay off the medical debt of everyone in California, New York, Texas, and Pennsylvania combined. “This is serious money that’s being misappropriated,” he says.
He singles out the Cleveland Clinic as an example. “Over the last three or so years, they received about $1 billion in taxpayer funds and tax breaks,” he says. “Of that, they pay 22 executives over $1 million apiece. I’m all for paying people fairly, but this is just not in keeping with a not-for-profit’s community mission.” Pitts adds that the remaining funds are often rolled into general coffers, not directed toward community care.
The structural issue, Pitts explains, is rooted in how hospitals are reimbursed. “They’re reimbursed by insurance—private and government—based on the services they provide, not the outcomes they deliver. It’s called fee-for-service. That’s completely upside down.” In contrast, Pitts notes, the pharmaceutical industry “figured out a long time ago they want to be reimbursed based on the value of their products.”
Hospitals, Pitts argues, are actively avoiding scrutiny. “They don’t want to be part of the conversation,” he says. “It’s hard to attack a local not-for-profit hospital when their names are on the backs of Little League uniforms.” But behind the charitable image, Pitts sees a system of self-interest and political protection. In New York, he notes, one hospital spent $34 million promoting itself to wealthy, insured patients instead of using that money for charity care. And across the country, nonprofits funnel “hundreds of millions of dollars a year in political contributions” to preserve their advantages.
“There’s a real need for transparency,” Pitts says, pointing out that hospitals are required by law to disclose pricing, but many simply ignore it. “There’s no oversight to really punish them,” he says.
Pitts warns that eroded public trust could have dangerous consequences. “When you leave these issues to the politicians, public trust and faith in not-for-profit hospitals erode. And when trust erodes—as it has with the FDA or CDC—bad things happen.” He adds that because nonprofit hospitals now focus their marketing on wealthier, better-insured patients, “they don’t want to deal with Medicare patients, they don’t want to deal with uninsured patients. It’s an absolute policy failure.”
But Pitts points out the possibility for improvements, such as through proposed legislation like the Holding Nonprofit Hospitals Accountable Act, sponsored by Rep. Victoria Spartz of Indiana. “Rather than creating the big beautiful bill that’s yesterday’s news, we have to legislate transparency and accountability,” Pitts says. “If people don’t see it, we’re not going to act on it.”
He also believes incentives must change. “You can’t just pay a fee for service anymore. You’ve got to pay for patient outcomes. This is common sense. Pharmaceuticals do it. Hospitals need to do it too.”
To drive reform, Pitts is shifting focus to the state level. “We’ve got to take this battle to the state level,” he says. “It’s easier to name and shame and get actions from state houses who are closer to the people.” He plans to publish state-specific reports detailing how individual nonprofit hospitals are failing their communities. “Transparency and accountability, realignment of incentives, making sure tax subsidies go where they’re supposed to, and keeping an eye on executive pay and political contributions—these are non-negotiable,” he says.