Dear Administrator McClellan:
The United States Senate Committee on Finance (Committee) has exclusive jurisdiction over the Medicare and Medicaid programs, and, accordingly, a responsibility to the more than 80 million Americans who receive health care coverage under these programs. As Chairman and Ranking Member of the Committee, we are responsible for oversight of the activities undertaken by the Centers for Medicare and Medicaid Services (CMS) in implementing and administering these programs, including the Medicare Part D prescription drug benefit. We write today seeking clarification and insight regarding CMS's administration and implementation of program integrity efforts for Medicare Part D.
On Jan. 1, 2006, a new era in the Medicare program began with the first prescriptions filled by prescription drug plans under Medicare Part D. With over 27 million Americans enrolled in the program and millions more enrolling each month, the message has gotten out that the Medicare Part D benefit is a good deal for those who are eligible. While this new benefit represents a giant leap forward providing meaningful prescription drug coverage for millions of Americans, it also represents an opportunity for fraud, waste, and abuse of taxpayer dollars.
To combat fraud in the Medicare Part D benefit, CMS publicly announced a new initiative within the Medicare Integrity Program (MIP) on October 7, 2005. This announcement outlined a three pronged approach, consisting of: data analysis, law enforcement cooperation, and consumer education. In implementing this comprehensive anti-fraud plan, CMS announced a contractual agreement between CMS and "eight Medicare Rx Integrity Contractors (MEDICs)" to work together in analyzing data, investigating potential fraudulent activities, conducting fraud complaint investigations, and developing cases for referrals to law enforcement for prosecution.
Through the use of various task orders, it was envisioned that CMS would delegate work to various MEDICs on both a national and regional level to facilitate Part D program integrity efforts.
In a briefing to committee staff on Nov. 22, 2005, program integrity officials from CMS stated that CMS has recognized 36 separate vulnerabilities that may exist in the implementation of the Medicare Part D benefit. Further, CMS stated that in order to best protect the Medicare program from the optimal starting period for MEDICs was Nov. 15, 2005.
Today, nearly five full months after the enrollment in the Part D benefit began and with three full months of Medicare outlays for the benefit, CMS has issued only one task order to a MEDIC for program integrity activities-the enrollment and eligibility national MEDIC (EEM). By continuing to allow months to pass without issuing any task orders to additional MEDICs, CMS has missed an opportunity to highlight program integrity activities during the early stages,
potentially leaving the Part D benefit vulnerable to fraud, waste, and abuse.
Recently, Congress acted to ensure that the MIP was adequately funded to cover the costs of establishing a comprehensive anti-fraud program by including $100 million for the MIP in the Deficit Reduction Act of 2005. This $100 million was provided to continue the work that the program integrity group had begun on Part D and was provided in addition to the $1 billion in administrative funds provided to CMS in the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA).
We are concerned that CMS has yet to fully implement the anti-fraud program. In the presentation given to committee staff in November, CMS stated the importance of the MEDIC program in detecting and preventing fraud and abuse stating, "With no MEDIC funding, CMS would have to rely on a staff of 8 people to perform fraud, waste and abuse work for the Part D program." Of further concern is the fact that with the additional $100 million in funding provided in the DRA, CMS is currently "meeting internally to determine the amount of funding that will be allocated to the MEDIC program." These statements, in conjunction with the fact that no new task orders have been issued by the MIP for the MEDICs, raise legitimate questions regarding CMS's implementation of anti-fraud activities for Medicare Part D.
Accordingly, as Chairman and Ranking Member of the Committee, we request that you provide the following documents and information:
(1) Provide a copy of the Part D fraud, waste and abuse guidance document which CMS provided to HHS/OIG, DOJ, and FBI on Nov. 18, 2005 for comment. In complying with this request please provide a copy of the document sent to these agencies and any comments that were received by CMS from the various agencies.
(2) Provide a copy of the list of "bad players" that was put together by CMS's program integrity group created following a review of prescription drug plan applications (as referenced by CMS program integrity staff at the Nov. 22, 2005 briefing).
(3) Provide a briefing for my Committee staff as soon as possible updating the Committee on anti-fraud activities for Medicare Part D.
We thank you in advance for your assistance with this matter by having your staff provide a point of contact for this matter no later than the close of business on April 19, 2006.
Additionally, we request that CMS provide a briefing on this matter as soon as possible and provide written responses and requested documents no later than April 28, 2006.
Sincerely,
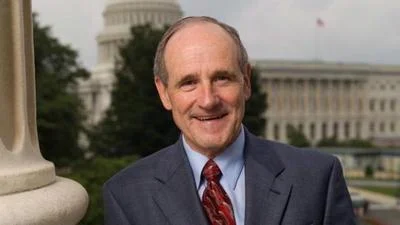
Charles E. Grassley Chairman
Max Baucus Ranking Member
Source: Ranking Member’s News